Published in Japan Forward 21/5/2020
In early April, the American embassy in Tokyo sent out a health alert urging its citizens to return to the United States as soon as possible. Insufficient testing for the coronavirus, the embassy warned, made the risk of infection in Japan “hard to read.”
At roughly the same time, friends in the UK repeatedly asked me if I was “safe” in Tokyo, given the Abe administration’s “mishandling” of the crisis as reported by the BBC.
The English language media had been scathingly critical of the Abe government’s approach, particularly the failure to implement draconian lockdown measures. There were flesh-creeping reports of a hypothetical worst case scenario in which Japan’s medical system would collapse, with 400,000 deaths and 800,000 patients on ventilators.
So far, the media doom-mongering has proved well wide of the mark. At time of writing, the cumulative total of reported coronavirus deaths in Japan is a mere 768, or 6 per million people.
In comparison, the figure for Britain, home of the BBC, is 526 deaths per million people. New York State, home to some of the loudest critics of Japan in the American media, has recorded 38x as many fatalities as the whole of Japan just by itself.
How is it possible that Japan’s coronavirus experience appears so mild compared to many Western countries? After all, the Japanese public does seems dissatisfied with the government’s handling of the pandemic, which was indeed hesitant at first and relies on social distancing and common sense, rather than compulsion.
Some observers have concluded that the Japanese numbers must be inaccurate, by accident or design. But, by concentrating on the performance of the government, are they looking in the wrong place? Is there something else going on?
Spanish Flu Sweeps the World
We have been here before – a hundred years ago, to be precise. Japan was ravaged by the deadly “Spanish Influenza” of 1918-19, but compared to many other countries the damage was limited. The government did indeed take a number of preventative measures, mostly copied from Western countries, but they were not rigorously enforced and some of them had little efficacy.
So how did Japan get off so lightly back then? Or was the whole thing a statistical mirage, created by undercounting?
The Spanish Influenza was the biggest health disaster of modern times. It spread through the world in three waves in the period after the First World War, probably carried by troop movements. It killed indiscriminately, claiming the young, the old and those in the prime of life.
Famous victims included Max Weber, the father of sociology, and painters Gustave Klimt and Egon Schiele. The worldwide death toll, which has been revised up significantly in recent years, is between 25-80 million.
In Japan, the final recorded death toll was at least twice that of the catastrophic Great Kanto Earthquake of 1923. One third of the population was infected and an estimated 250,000-480,000 were killed by the virus. Victims ranged from the brilliant young painter Kaita Murayama to Hogetsu Shimamura, the leader of Japan’s modern theater movement.
In the early twentieth century, viruses travelled by ship and train, but that was enough to spread the disease far and wide. The Spanish Flu arrived Japan in the spring of 1918 and was killing people in rural prefectures such as Fukushima and Yamanashi by August. In the rapidly expanding mega-cities of Tokyo and Osaka, large families were packed together in cramped tenements – ideal conditions for the virus to spread.
The influenza virus was not discovered until 1933, so much about the pandemic remains obscure. Two historians from the University of Canterbury in New Zealand, Geoffrey Rice and Edwina Palmer, have made a valiant effort to assess the scale of the disaster in Japan and the effectiveness of government policy.
Their conclusion is that Japan fared far better than other non-Western countries and probably better than many European countries too.
Selected Mortality Rates: Spanish Influenza (1918-19), deaths per 1,000
Australia 2.3
Ireland 4.04
Japan 4.5
Canada 5.0
USA 5.2
England and Wales 5.8
Sweden 5.9
Switzerland 6.0
Spain 8.3
Italy 10.6
Indonesia 17.7
Mexico 23
Nigeria 30
India – central provinces 67
Alaska (native peoples) 80
Western Samoa 220
Source: Rice / Palmer, Pandemic Influenza in Japan
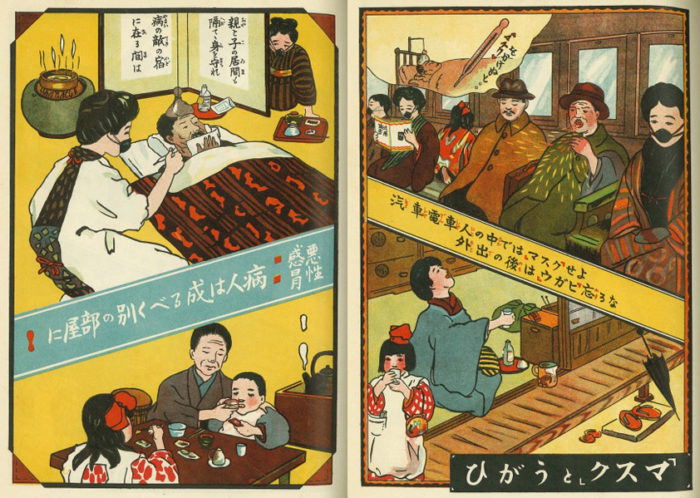
How much of this relative success was due to Japanese government policy? Rice and Palmer note that the government’s advice was sensible, with stress on mask-wearing, gargling and anti-pneumonia vaccination, which was effective against often fatal secondary infections.
As with coronavirus today, there was no cure or anti-virus vaccine. Home rest with plenty of fluids was good advice, but the authorities did not close cinemas and theatres, as was the case in some foreign cities, and neither did they recommend sponging to reduce fever, which could be crucial in saving lives.
Furthermore, the number of doctors and hospitals was low in relation to population. As Rice and Palmer put it, “the vast majority of flu cases were nursed by amateurs, close family, or neighbours” – at home, because there was nowhere else to go.
Rather than ascribing Japan’s low mortality to governmental activity, Rice and Palmer offer two alternative explanations. The first is a degree of “herd immunity” conferred by the earliest, and less dangerous wave of infection in the spring of 1918.
The second is the community response – fastidious hygiene, the quality of home nursing, use of traditional medicines with some efficacy in reducing fever and headaches. In their willingness to use masks, Rice and Palmer note, the Japanese showed themselves “far more alert to the dangers of droplet infection” than Europeans in 1918.
Back to the Future
Rice and Palmer’s work has not gone unchallenged. The late Akira Hayami, Professor Emeritus at Keio University, estimated Japanese fatalities from the pandemic at 450,000, including flu sufferers who died from other causes. Another group, led by S.A. Richard of the National Institute of Health in the U.S., takes the total up to 480,000, adding in the victims of a fourth wave in 1920, which is often reckoned a separate strain due to pathogenic drift.
More controversially, in 2013 Professor Siddartha Chandra of Michigan State University produced a statistical model based on long-term demographics that increases Japanese deaths sevenfold, to levels similar to Mexico and Nigeria. In turn, Chandra’s methodology was rubbished in 2016 by Japanese researchers Hidekazu Nishimura and Yasushi Ohkusa.
If the complexion of a century-old pandemic is still disputed, it is more than likely that the controversies relating to the coronavirus will rumble on for decades to come. Indeed, some of the issues are the same. What are the most efficacious treatments? Do masks work? How much compulsion is justified? How reliable are the statistics – are we comparing apples with mikan?
And perhaps the most salient lesson of the Japanese experience – which has the bigger influence on outcomes, government policy or community-level behaviour?
Meanwhile we continue with our masks, hand-washing and various forms of quarantine – anti-virus strategies that would have been familiar to our great grandfathers and grandmothers a century ago.